Fall 2023 - Current Issue Pedaling With Intention
How Yoseph Assefa ’16, CEO of Leafy Bikes, created a brand that combines profit and purpose.
Also on this issue:
- How AI Can Better Healthcare
- The Legacies of Barry
- The Future of DE&I in Corporate America
All Issues
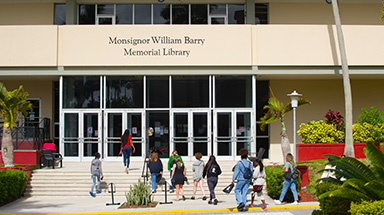
Barry University Magazine is published twice a year by the Office of Institutional Advancement. The contents of this magazine are selected to reflect the University’s core commitments, to demonstrate the range of great work taking place on its campuses and in the community, and to provide news about the University and its alumni.